COVID Case Numbers Seesaw Through Weekend
Hospitalizations remain fairly flat, but new cases of COVID-19 vacillated over the weekend. As schools begin discussing when students should return to campus, the county has begun to see an uptick in cases among children, as well. We have today’s bullet points:
- COVID case numbers seesaw through weekend;
- Abbott announces automatic SNAP renewals will continue;
- United States of Care releases recommendations for CARES 2 package.
COVID Case Numbers Seesaw Through Weekend
A total of 2,726 new cases of the novel coronavirus were reported by Dallas County health officials between Friday and Sunday, and an additional 28 deaths, bringing the county’s total cases up to 46,813, including 605 confirmed deaths.
For reference, last Sunday, the total case count was 41,266, and 525 deaths.
The numbers seesawed a bit through the weekend. On Friday, the county reported 659 new cases and nine deaths; on Saturday, 1,267 new cases and 18 deaths; and on Sunday 800 new cases and one death.
Among the dead was a 5-year-old Dallas boy with underlying high-risk health conditions. The county reported that more than 1,450 children 18 and younger have been diagnosed with COVID-19 during the first three weeks in July, including 29 children who were hospitalized during that time. There have been more than 98 confirmed cases in children and staff from 65 separate daycares in Dallas County since June 1, including three staff members that were hospitalized.
“This is our first pre-teen death here in Dallas County. I want to point out to the public that we have seen a sharp uptick in children getting COVID,” Dallas County Judge Clay Jenkins said Friday. “We currently have over 1,450 children under age 18 who’ve tested positive since July 1. Parents, it’s imperative that children, like everyone else, follow the guidelines to stay safe.”
Also among the dead are a Dallas man in his 30s with underlying conditions, a Duncanville man in his 40s, a Dallas man in his 40s with underlying health conditions, a Grand Prairie man in his 40s with underlying health conditions, a Grand Prairie man in his 50s with underlying health conditions, an Irving man in his 50s with underlying health conditions, a Dallas man in his 50s who was found dead at his home, a Dallas man in his 60s, a Lancaster man in his 60s with underlying conditions, a Dallas woman in her 60s with underlying conditions, a Garland man in his 60s with underlying health conditions, a Dallas man in his 70s with no underlying conditions, a DeSoto woman in her 70s with underlying conditions, a Garland man in his 70s with underlying conditions, a Dallas woman in her 70s with underlying conditions, a Dallas man in his 70s with no underlying conditions, a Mesquite man in his 70s with no underlying conditions, a Dallas woman in her 80s with underlying conditions, and a Dallas man in his 80s with no underlying conditions.
Long-term care facilities continue to account for a third of all COVID-19 deaths, including a man in his 50s who died at the Dallas facility he lived at, a man in his 60s who lived at a DeSoto facility, a man in his 60s who lived at a Cedar Hill facility, a woman in her 70s who died at the Dallas facility she lived at, a man in his 70s who died at the Dallas facility he lived at, a man in his 80s who lived at a DeSoto facility, a woman in her 80s who died at the Dallas facility she lived at, and a woman in her 90s who died at the Dallas facility she lived at.
Saturday, Jenkins said the additional 18 deaths that day made it the “deadliest week thus far.”
“We will see improvements if we continue to wear our masks whenever outside our home and if we avoid unnecessary trips and any establishment where a mask cannot be worn one hundred percent of the time,” he said. “This includes in-restaurant dining; however, our restaurants are at a critical point. With PPP having run out and most people following the health advice and not eating in dining rooms, restaurant revenues are dropping off. If you’re able, please order take-out and delivery from our restaurants to support them and the people that they employ.”
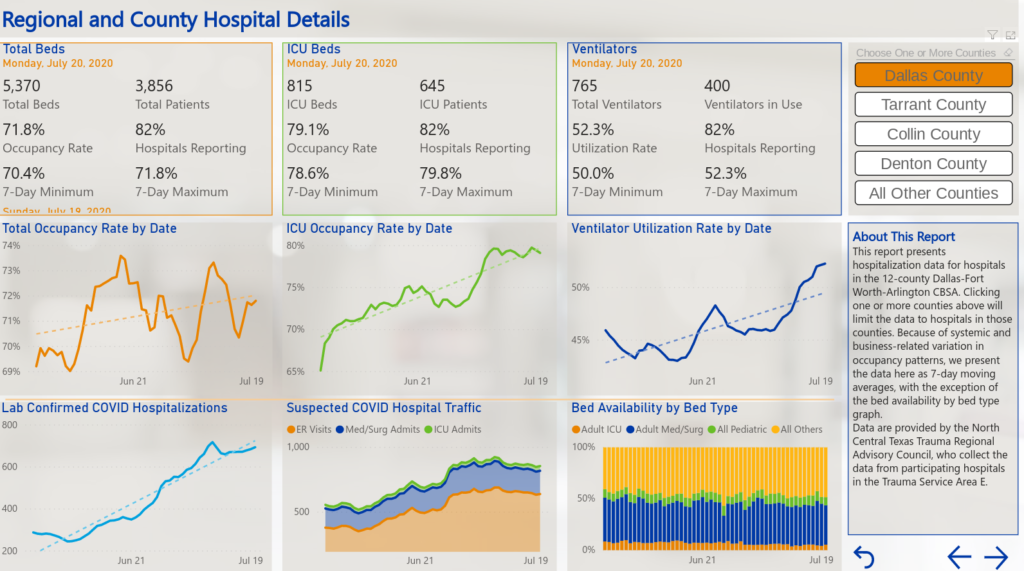
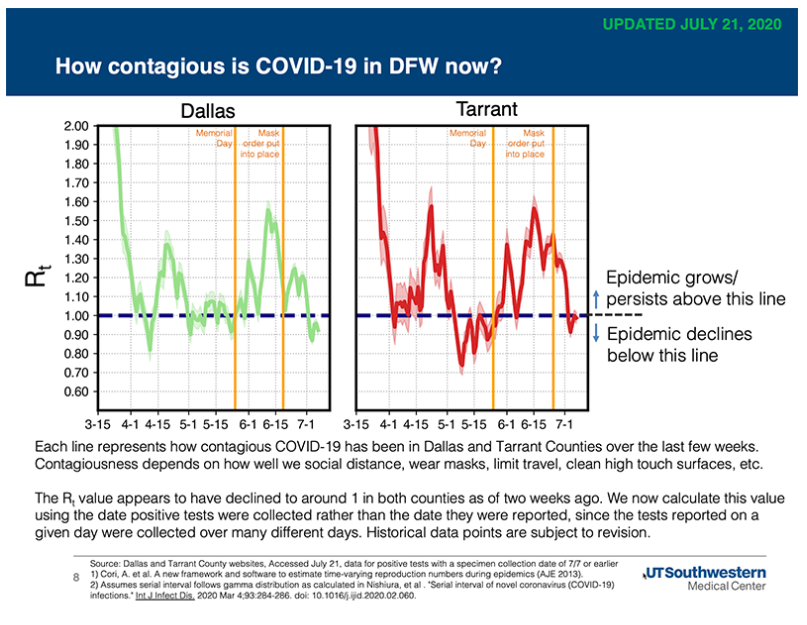
Sunday data from the Institute for Urban Policy Research, which collects data from the North Central Texas Trauma Regional Advisory Council, shows in Dallas County, roughly 82% of hospitals are reporting, and the occupancy rate is somewhere around 72%, but almost 80% of all available ICU beds are in use, and about half of all ventilators are in use.
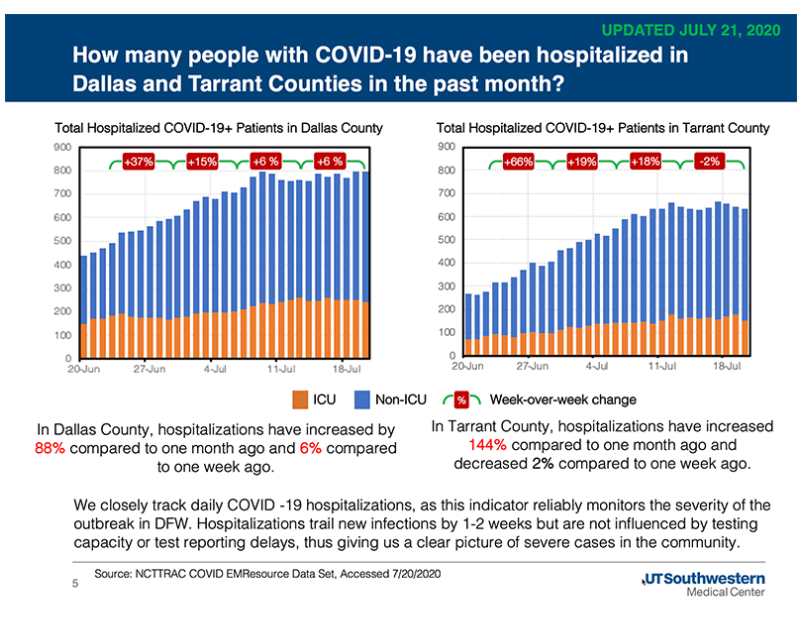
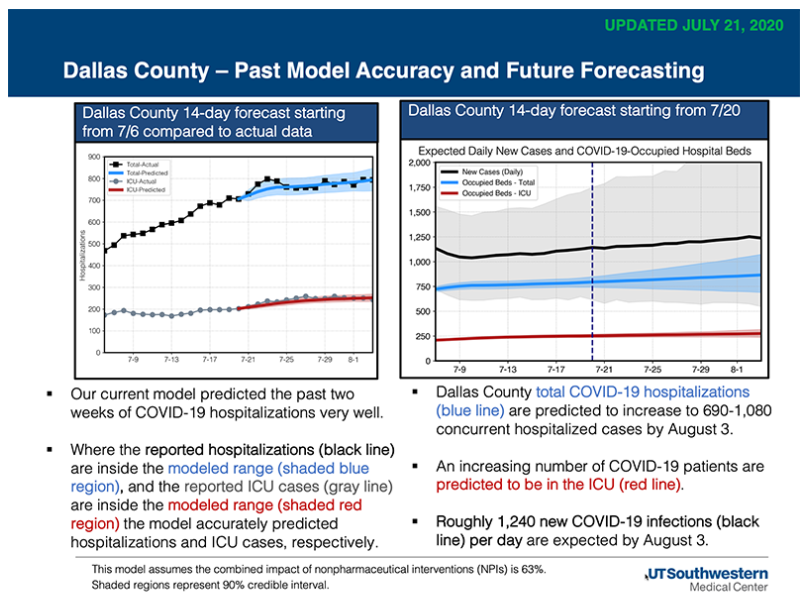
UT Southwestern’s latest forecast projects that by August 3, Dallas County hospitals could see concurrent hospitalizations from COVID-19 increase to between 690 and 1,080 cases. Hospitalizations in the Dallas-Fort Worth area have increased by 2% in a week, and 107% compared to a month ago. In Dallas County, hospitalizations have increased by 6% in a week and 88% compared to a month ago.
In the county’s July 21 aggregate report, most cases continue to be between the ages of 18 and 60, with the 18-40 age group accounting for 47% of the cases, and the 41-64 age group accounting for another 34% of the total cases.
Close contact or community transmission continues to be the biggest risk factor for contracting COVID-19, accounting for roughly 91% of all cases. Being incarcerated in a federal prison, living in a long-term care facility or being incarcerated in the county jail are a distant second, third, and fourth, at 2.7%, 2.4% and 1.5%, respectively.
Of the testing done, positive cases accounted for 26.8% as of July 11, with 1,952 positives coming from 7,282 tests. Testing and positive test results of COVID-19 far outpaces any other respiratory virus – even if you combine them all.
Twelve percent of all cases ended up hospitalized – 21% ended up in intensive care, and 12% ended up on a ventilator.
In a city-by-city breakdown, Dallas still comes in with the highest number of cases – 23,055, or 53.6%. Highland Park has 39 (up from 36 Sunday) cases so far, and University Park has 72 (up from 64).
Abbott Announces Automatic SNAP Renewals Will Continue
Gov. Greg Abbott Friday announced that the Texas Health and Human Services Commission has received federal authority to extend certifications by six months for Supplemental Nutrition Assistance Program (SNAP) recipients whose benefits are up for renewal in July and August. HHSC received federal approval from the U.S. Department of Agriculture to also waive interview requirements for new and current households.
“The State of Texas is committed to ensuring families have access to nutritious food throughout the COVID-19 pandemic,” said Abbott. “By extending automatic SNAP renewals and temporarily waiting interview requirements, we will ensure more Texans have healthy meals for their families. I thank our federal partners for their continuous support as we respond to COVID-19.”
“As we continue to fight against COVID-19, these automatic renewals provide food security and peace of mind to families in need during this unprecedented time,” said Texas HHS Access and Eligibility Services Deputy Executive Commissioner Wayne Salter. “Waiving interviews also reinforces that it is important to stay home when possible to minimize potential exposure to COVID-19.”
The interview waiver applies to new applicants as well as those whose benefits are up for renewal, and HHSC can process applications as they are received and make eligibility determinations faster.
The automatic renewals will extend the benefits of approximately 276,000 households who have not yet turned in their renewal information for July and August. This extension is the latest change to SNAP since the onset of COVID-19. Other initiatives include the SNAP Online Purchasing Pilot, Pandemic EBT, and allowing the maximum, allowable amount of SNAP benefits by household size.
Texans in need can apply for benefits, including SNAP and Medicaid, at YourTexasBenefits.com.
United States of Care Releases Recommendations for CARES 2 Package
Friday five entities with a shared mission of providing accurate information and data regarding the transmission of the novel coronavirus held a webinar to discuss new data on COVID-19 surges, mask efficacy, and the new federal policy that requires data be sent to the White House instead of the CDC.
The webinar, conducted by CovidExitStrategy.org, United States of Care, Resolve to Save Lives, Covid19StatePolicy.org, and the Duke-Margolis Center for Health Policy can be viewed here. Llisten to the audio here.
“At United States of Care, we have found that Americans want accurate and reliable data to keep themselves and their loved ones safe. Covidexitstrategy.org provides that need, by supplying real-time data on where their state stands in the battle against COVD-19,” stated Emily Barson, United States of Care executive director. “As a policy organization, we outlined our recommendations for the next COVID-19 relief package being debated on Capitol Hill and, with a group of other organizations, we sent a letter advocating for more resources for contract tracing. Accurate and timely data must be used to inform the public and policymakers on how to combat COVID-19 and prepare for the fall flu season,” added Barson.
CovidExitStrategy.org was founded by a group of public health and crisis experts, with previous experience working at the White House, Department of Health and Human Services, and on the Ebola epidemic in West Africa. COVID Exit Strategy is a non-partisan group of experts who have worked across multiple administrations.
“Last week, we lost access to a critical indicator: the utilization and availability of intensive care and inpatient beds by each state. This happened because hospitals were instructed to report data to a new system developed by HHS called HHS Protect. The data feeds were returned within the week, but we are seeing inconsistencies in the data. We hope those are resolved soon, so we can continue to incorporate that data.” said Ryan Panchadsaram, co-founder of CovidExitStrategy.org. “The new HHS Protect system incorporates 200 datasets. Currently only 2-3 categories of data are being made available to the public. It is critical that the public has access to all COVID response related data.”
“We are lacking key data on testing, such as test turnaround time, to understand if isolation and quarantine strategies can be effective to control disease. We don’t know how any state is doing with respect to contact tracing. Most don’t report any information on essential indicators related to contact tracing programs. We need more publicly available, standardized data across the country to understand patterns of disease and effectiveness of our response” remarked Cyrus Shahpar of Resolve to Save Lives.
“As we look at COVID-19 raging in the Sunbelt states, we need to remember that there States in the North East that not only have been successful in lowering previously high case levels, but have also managed to prevent a resurgence of cases after reopening. We can and should learn from those states,” said Marta Wosinska, deputy director at the Duke-Margolis Center for Health Policy.
“With many new orders issued over the last four weeks, 30 states and DC now have strict, statewide mandates to wear masks at least in indoor public spaces. This means more than 70% of Americans live under these statewide orders. However, a large number of current “hotspot” states like Florida, Georgia, and Arizona still lack sufficiently broad statewide mandates.” added Christopher Adolph of Covid19StatePolicy.org. A summary of the timing of statewide mask mandates across the United States is here.
As part of the call, USofCare also outlined their recommendations for the next COVID-19 relief package being presented to Congress, and a letter with the American Medical Association and other business, and medical and service groups that advocates for more resources for contract tracing.