Does Your Blood Type Affect Whether You Get COVID-19?
As data from other countries and regions who have been dealing with COVID-19 and have even flattened the curve begins to be analyzed, new potential treatments and clues about how the virus impacts people is continuously revealed. We take a look at one potential clue, and more in today’s bullet points.
- Preliminary studies indicate blood type may be a risk factor in COVID-19;
- New cases continue to rise, including in the Park Cities;
- PUC extends electricity relief program through August.
Does Your Blood Type Affect Whether You Get COVID-19?
Several studies have shown preliminary evidence that blood type may be a factor in how severe a bout of COVID-19 may be.
The first hint that blood type might have a bearing on whether or not someone with the virus lands in the hospital was found in China in March. Researchers there found that by comparing COVID patients in three hospitals in the area hardest hit with people who were not hospitalized, they found that people with Type A blood had a greater risk of landing in the hospital, while people with Type O had a lower risk.
In fact, Type A people had a 21% greater risk, and Type O had a 33% lower chance of hospitalization.
“The results showed that blood group A was associated with a higher risk for acquiring COVID-19 compared with non-A blood groups, whereas blood group O was associated with a lower risk for the infection compared with non-O blood groups,” the researchers said.
In April, researchers at Columbia University performed similar research on 1,559 people who were tested to see if they had the coronavirus that causes COVID-19. That small-scale study found that Type A people had a 34% greater chance of testing positive, and Type O people had a 20% lower chance of testing positive.
“We found a higher proportion of blood group A and a lower proportion of blood group O among COV+ patients compared to COV-, though in both cases the result is significant only in Rh-positive blood types,” the Columbia researchers said, adding that their findings regarding hospitalizations were similar to the Chinese study.
The most recent research, published in June in the New England Journal of Medicine, found that having Type A blood seemed to increase risk of having COVID-19 badly enough to require hospitalization by 45%, while having Type O blood appeared to reduce risk by 35%.
The researchers from Germany and Norway looked at genetic data from about 1,600 patients hospitalized in Italy and Spain, and compared them to roughly 2,200 people who didn’t have the virus, adjusting for age and sex, the findings held up even when they separated the patients by whether they were from Italy or Spain.
“While more research is needed to pinpoint the precise underlying genes and mechanisms responsible, a recent genome-wide association (GWAS) study, just published in the New England Journal of Medicine, finds that gene variants in two regions of the human genome are associated with severe COVID-19 and correspondingly carry a greater risk of COVID-19-related death,” wrote National Institutes of Health director Dr. Francis Collins, regarding the study. “The two stretches of DNA implicated as harboring risks for severe COVID-19 are known to carry some intriguing genes, including one that determines blood type and others that play various roles in the immune system. In fact, the findings suggest that people with blood type A face a 50 percent greater risk of needing oxygen support or a ventilator should they become infected with the novel coronavirus. In contrast, people with blood type O appear to have about a 50 percent reduced risk of severe COVID-19.”
Does this mean that if you’re a Type O you can be less diligent about social distancing and mask wearing? Researchers say no, it just means that the research may help provide some diagnostic and treatment tools to help prevent and combat the disease.
“The hope is that these and other findings yet to come will point the way to a more thorough understanding of the biology of COVID-19,” Collins wrote. “They also suggest that a genetic test and a person’s blood type might provide useful tools for identifying those who may be at greater risk of serious illness.”
New Cases Continue to Rise, Including in the Park Cities

A total of 3,270 new cases of the novel coronavirus were reported by Dallas County health officials between Friday and Sunday, and an additional 24 deaths, bringing the county’s total cases up to 41,266, including 525 deaths.
For reference, last Sunday, the total case count was 33,800, and 451 deaths.
On Friday, the county reported 1,195 new cases and 13 deaths; on Saturday, 1,031 new cases and nine deaths; and on Sunday 1,044 new cases and two deaths.
Among the dead are a Grand Prairie man and woman – both in their 20s, a Dallas man in his 30s, an Irving man in his 50s, a Dallas man in his 50s, a Dallas man in his 60s, a Lancaster woman in her 60s, a Garland man in his 60s, a Grand Prairie man in his 70s, a Mesquite man and woman – both in their 70s, two Dallas men in their 70s, a Rowlett man and woman – both in their 70s, an Irving woman in her 70s, a Dallas man in his 80s, a Rowlett man in his 80s, a Garland woman in her 80s, a Richardson woman in her 90s, and a Dallas man in his 90s.
Additionally, a Dallas man in his 70s with underlying high risk health conditions died in an area hospital emergency room, and a man in his 60s who was an inmate at a Seagoville correctional facility died at an area hospital.
Long-term care facilities continue to account for a third of all COVID-19 deaths, including a man in his 90s who was a resident of a Dallas facility.
“This was our deadliest week in Dallas County for COVID-19. We had a total of 74 deaths reported compared to last week’s record of 54. This week we saw a drop in our average daily number of new cases by 36, with 1,085 as the daily average this week versus last week’s record of 1,121 average daily cases,” said Dallas County Judge Clay Jenkins Saturday. “Our COVID-19 hospitalizations, ER visits and ICU admissions were near record levels this week as well. All this is strong indication that you should wear a mask when outside your home and avoid any business where masks are not being worn 100% of the time.”
The county said that the average number of COVID-19 hospitalizations Friday was 794 patients. Emergency room visits also continued to increase, representing about 33% of all ER visits, according to information reported to the North Central Texas Trauma Regional Advisory Council.
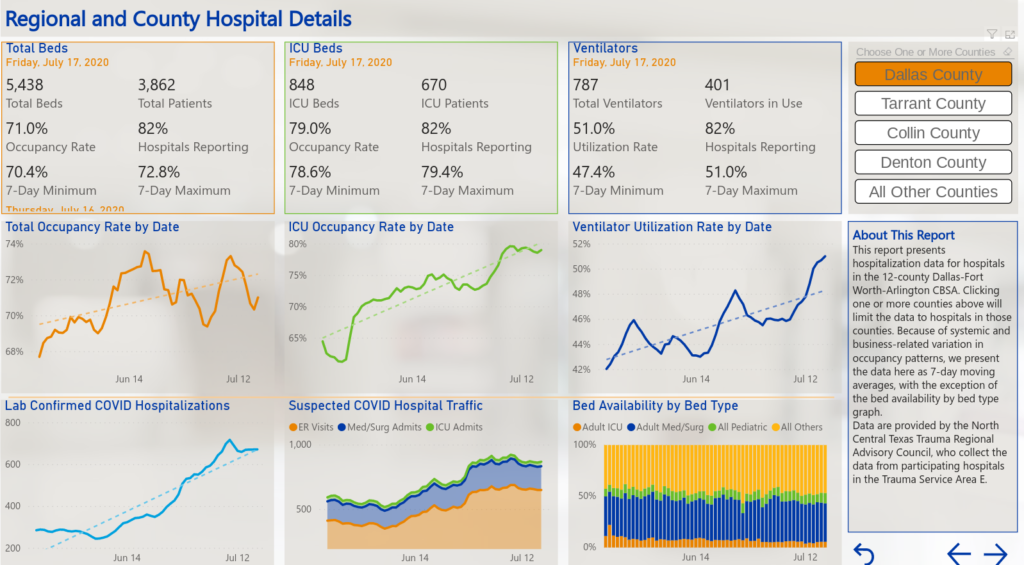
What does that mean for hospitalizations? By looking at the Sunday data from the Institute for Urban Policy Research, which collects data from the North Central Texas Trauma Regional Advisory Council, we can see that for Dallas County, roughly 82% of hospitals are reporting, and the occupancy rate is somewhere around 71%, but almost 80% of all available ICU beds are in use, and a little more than half of all ventilators are in use.

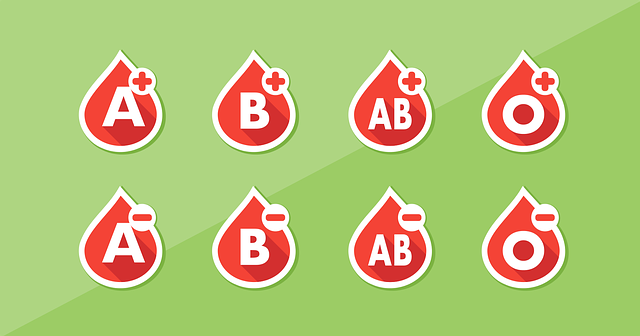
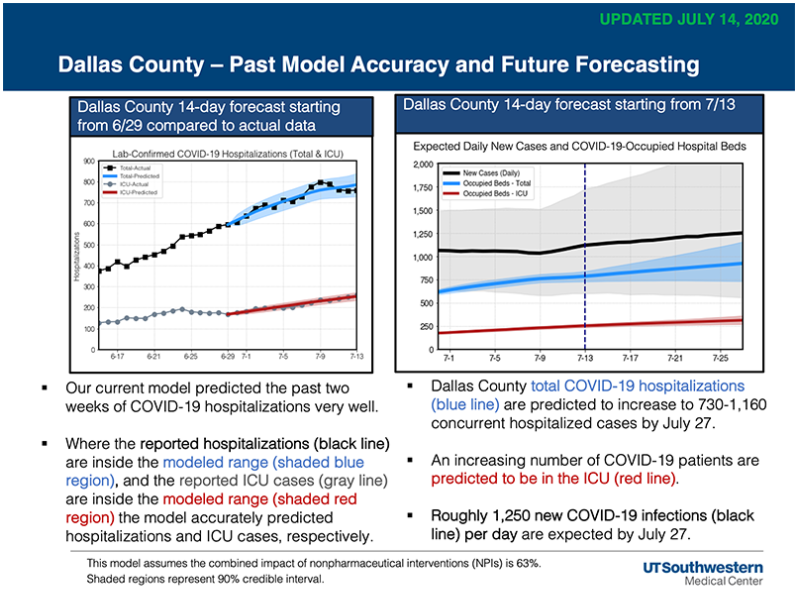
UT Southwestern’s latest forecast projects that by July 27, Dallas County hospitals could see concurrent hospitalizations from COVID-19 increase to between 730 and 1,160 cases. Hospitalizations in the Dallas-Fort Worth area have increased by 8% in a week, and 158% compared to a month ago. In Dallas County, hospitalizations have increased by 3% in a week and 101% compared to a month ago.
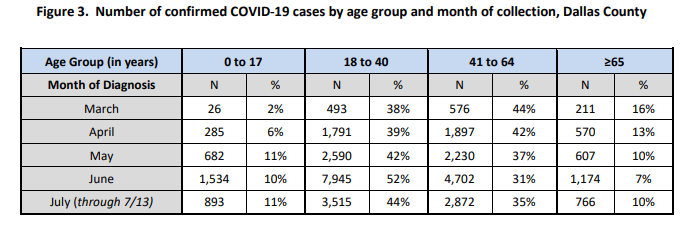
In the county’s July 17 aggregate report, most cases continue to be between the ages of 18 and 60, with the 18-40 age group accounting for 47% of the cases, and the 41-64 age group accounting for another 34% of the total cases.
Close contact or community transmission continues to be the biggest risk factor for contracting COVID-19, accounting for roughly 91% of all cases. Being incarcerated in a federal prison, living in a long-term care facility or being incarcerated in the county jail are a distant second, third, and fourth, at 2.7%, 2.4% and 1.5%, respectively.
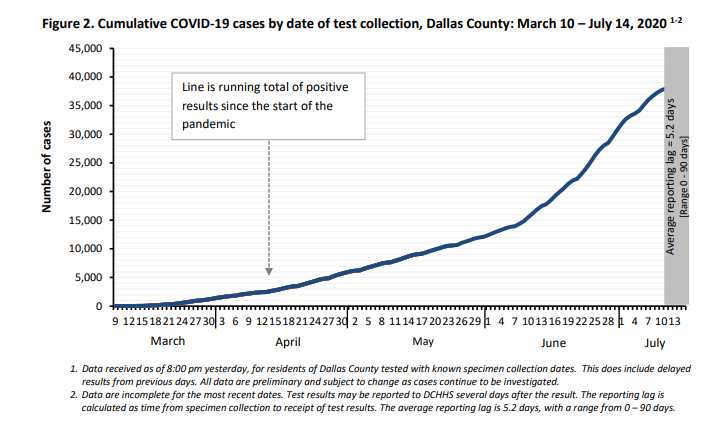
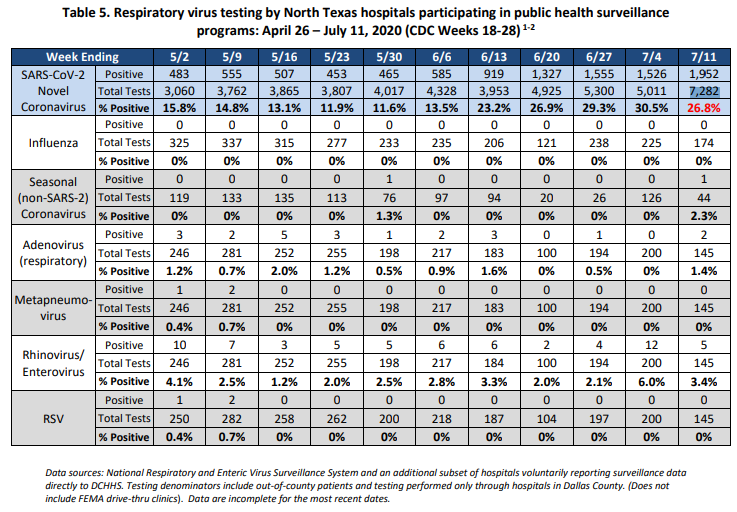
Of the testing done, positive cases accounted for 26.8% as of July 11, with 1,952 positives coming from 7,282 tests. Testing and positive test results of COVID-19 far outpaces any other respiratory virus – even if you combine them all.
Twelve percent of all cases ended up hospitalized (compared to 11% last Sunday) – 22% ended up in intensive care, and 12% ended up on a ventilator.
In a city-by-city breakdown, Dallas still comes in with the highest number of cases – 21,163, or 54%. Highland Park has 36 (up from 28 last Sunday) cases so far, and University Park has 64 (up from 55).
PUC Extends Electricity Relief Program Through August

Texas Public Utility Commission will extend the state’s Electricity Relief Program to August 31, 2020.
Citing the governor’s July 10 decision to extend the COVID-19 disaster declaration for all Texas counties, the orders extend the protection from disconnections for non-payment for ERP participants, continues the requirement for retail electric providers to offer deferred payment plans when requested, and sets August 31, 2020 as the last day for enrollment in the ERP.
“This pandemic is far from over, so we will continue to monitor its impact on Texas utility customers as we follow the governor’s lead on assisting the Texans who need it most,” said chairman DeAnn Walker. “Our goal is to ensure our state emerges from these troubled times with our competitive electricity marketplace intact and its benefits positively affecting customers across the state.”
“Regulatory certainty is a hallmark of the Texas model and we’re doing our best to keep everyone in the equation informed as to our intentions,” said commissioner Arthur D’Andrea. “The entities under our purview have worked hard to respond to our guidance and I expect they’ll continue to do so for the duration of the ERP.”
Initially created by commission order on March 26, the ERP is intended to help unemployed customers of retail electric providers by providing protection from disconnections for non-payment and offering bill payment assistance using funds from a rider charge applied to the bills of electricity customers across ERCOT.
Counting Texans in the program due to their inclusion on the state’s low-income list (due to participation in SNAP or MEDICAID), the ERP program is currently protecting more than 590,000 households from disconnection for non-payment.
“I’m proud that this commission has adapted to emerging challenges while remaining sensitive to consumer concerns,” said commissioner Shelly Botkin. “I appreciate everyone working together to find solutions.”
Texas electricity customers in the areas of the state open to retail competition who have filed or will file for unemployment with the Texas Workforce Commission can request enrollment in the program at http://TXCOVID19ERP.org or call 866-454-8387 until August 31.