Are We Any Good at Social Distancing?
As everyone watches anxiously to see if a predicted second surge will happen, and if the county is truly plateauing and ready to see cases of COVID-19 decline, a lot happens every day. Here are your bullet points for the day.
- Are we any good at social distancing?
- New cases remain flat, but death toll climbs by 14
- St. Marks students making PPE, but need help
Are We Any Good At Social Distancing?
 You may recall on Monday we talked about how many lives were saved, and how many hospitalizations were avoided, as calculated by the Big Cities Health Coalition. Nationally, it said, counties and cities that adopted shelter-in-place and safer-at-home orders early may have attributed to avoiding about 2.1 million hospitalizations, and saving over 200,000 lives.
You may recall on Monday we talked about how many lives were saved, and how many hospitalizations were avoided, as calculated by the Big Cities Health Coalition. Nationally, it said, counties and cities that adopted shelter-in-place and safer-at-home orders early may have attributed to avoiding about 2.1 million hospitalizations, and saving over 200,000 lives.
Dallas County, BCHC said, avoided more than 113,500 hospitalizations and 11,876 deaths.
But Unacast, a verified human mobility data company, is doling out grades on social distancing – and it doesn’t look so good for Dallas County, or Texas, for that matter. Both the county and the state got a big, fat “F” for social distancing. You can see the scorecard for the county here.
The company explains in-depth here the methodology, but basically they’re tracking three things: Average distance traveled now versus before the pandemic, average non-essential trips now versus pre-COVID-19, and human encounters.
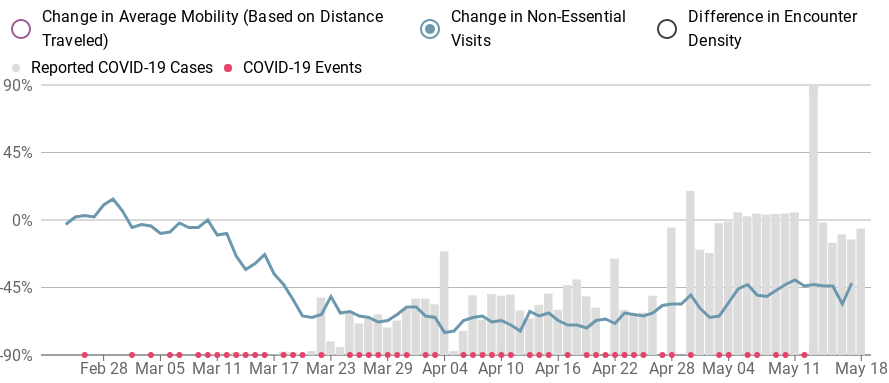
“Several of our Scoreboard users observed something that was on our radar: in many rural places and other less-populated areas, the baseline for ‘social distancing’ is naturally much lower and thus, it is inaccurate to apply the same standard to places that have drastically less potential to decrease. We heartily agree,” the company explained.
“Moreover, since the virus itself is spread via person-to-person contact, we needed to incorporate some notion of that into our score,” it continued. “Since our data cannot detect if two humans have actually met, we instead use our data to simulate potential encounters and derive the probability that two devices that were in the same place at the same time.”
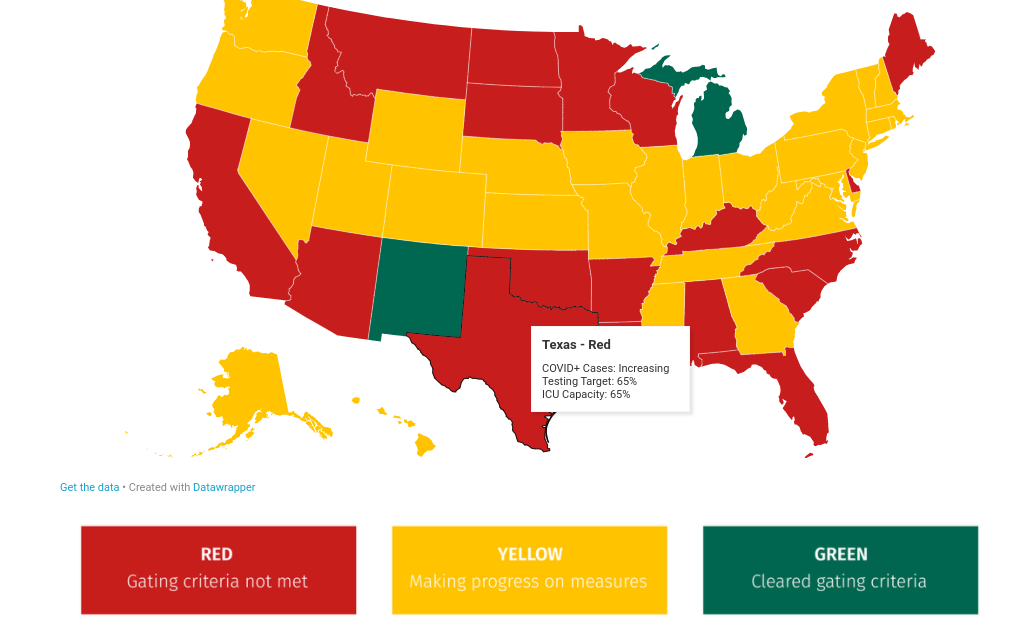
We also found another new tool created by public health experts – CovidExitStrategy.org. The nonpartisan group is compiling data and comparing it to the White House’s own criteria for safe reopening of business to show when states are actually nearing the “gating criteria.”
“For this site, we are using the gating criteria provided by the White House. In their Reopening America Again guidelines. The document does not specifically identify data sources or measures, so we had to translate what those meant,” the group said.
From there, they assigned states a color based on how close they are to reaching the gating criteria. States can come close, then go back to red, or even go green and go back to yellow or red, based on the most recent data, as you can see from the explainers beneath the map on the website.
Here’s Texas:
New Cases Remain Flat, But Death Toll Climbs by 14
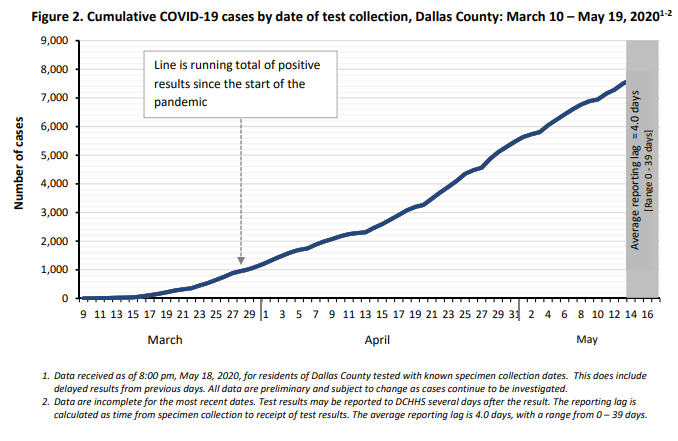
The curve seems to be possibly flattening when it comes to new cases, with Dallas County health officials reporting 225 new cases of COVID-19 Tuesday, bringing the total number of cases in the county to 7,904.
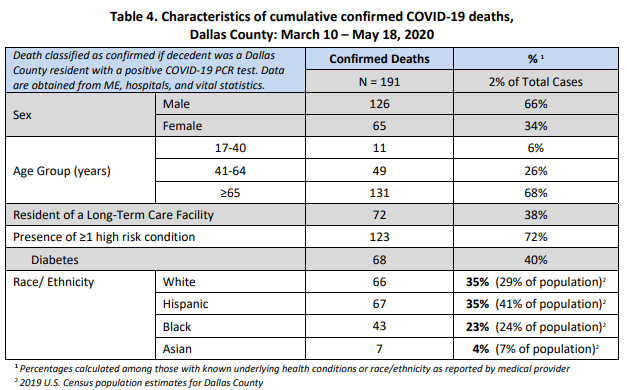
The county also reported 14 deaths Wednesday – by far the biggest daily death toll since the pandemic hit the county in March. The additional deaths bring the county death toll to 191.
The dead include several who died at area hospitals, including a Dallas man in his 40s, a Grand Prairie man in his 50s, a Grand Prairie woman in her 50s, a Dallas man in his 60s, an Irving woman in her 60s, an Irving man in his 70s, a Duncanville man in his 80s, and a Garland woman in her 90s. A Dallas man in his 50s was found dead at his home.
Five of the deceased were residents of long-term care facilities, including a Mesquite woman in her 60s, a Mesquite man in his 60s, a Dallas man in his 60s, and an Irving woman in her 70s. A man in his 90s died at the Mesquite long-term care facility he lived in.
Of cases requiring hospitalization, two-thirds have been under 65 years of age, and about half do not have high-risk chronic health conditions. Diabetes has been an underlying high-risk health condition reported in about a third of all hospitalized patients with COVID-19. Of the 191 total deaths reported to date, over a third have been associated with long-term care facilities.
“Today is our most deadly day thus far during the COVID-19 crisis as we report the passing of 14 of our residents. Additionally, we have 225 more positive cases,” said Dallas County Judge Clay Jenkins. “All this illustrates the importance of you avoiding crowds whenever possible, maintaining a 6-foot distance at all times from people outside your household, wearing a cloth face covering at businesses and on public transportation, as well as practicing good hygiene.”
“As the Governor opens more and more businesses, it’s important that each of us focus not on what is legal, but also focus on what is safe and the recommendations of the public health committee,” Jenkins said, pointing to the county’s website, www.DallasCountyCOVID.org.
In his evening newsletter, Dallas Mayor Eric Johnson said that 25 hospitals reported their bed availability Tuesday. Of the 5,713 total beds, 62% are occupied. Of the 826 ICU beds available, 68% (or 562) are occupied. And 325 of the total 945 ventilators available are currently in use.
Of cases requiring hospitalization who reported employment, about 80% have been critical infrastructure workers including those in healthcare (18%), transportation (16%), food and agriculture – which includes grocery stores and places you can buy food (15%), public works (8%), finance (5%), communications (4%), teachers, real estate, and clergy (8%), and first responders (3%).
In the county’s May 19 aggregate report, most cases continue to be between the ages of 18 and 60, with the 18-40 age group accounting for 40% of the cases, and the 41-64 age group accounting for 41% of the total cases.
Close contact or community transmission continues to be the biggest risk factor for contracting COVID-19, accounting for almost 86% of all cases. Living in a long-term care facility, being incarcerated in the county jail, and domestic travel are a distant second, third, and fourth, at 5.2%, 4.2%, and 1.6%, respectively. Creeping up, though, are cases from meat and food processing facilities, which now account for 1.3% of all cases in the county.
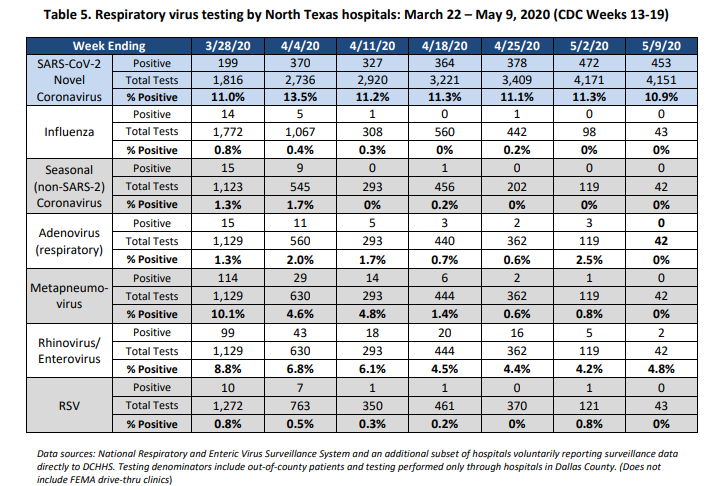
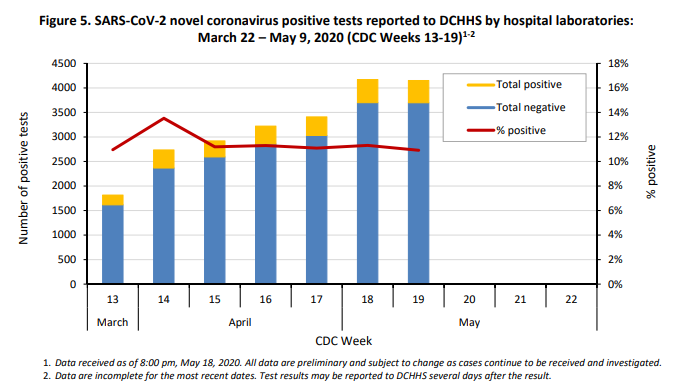
Of the testing done, positive cases accounted for 10.9% of tests at local hospitals as of May 9, down slightly from 11.3% as of May 2, with 453 positives coming from 4,151 tests. However, testing and positive test results of COVID-19 far outpaces any other respiratory virus – even if you combine them all.
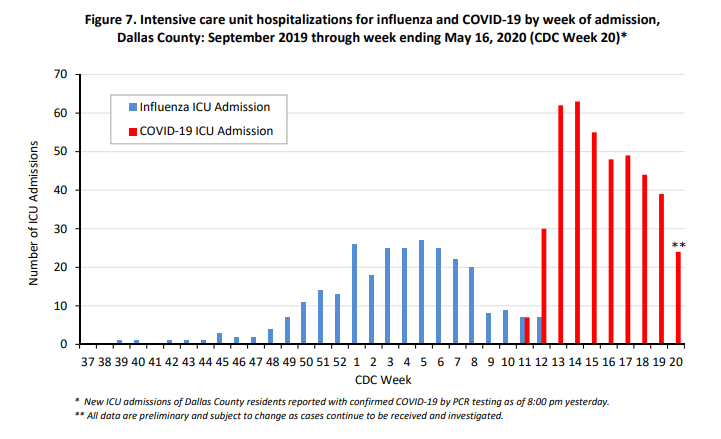
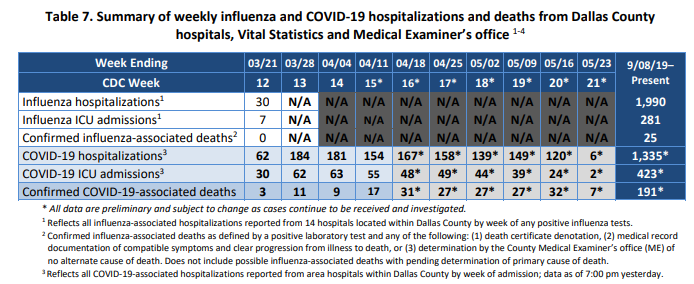
Hospitalizations because of COVID-19 have also eclipsed influenza hospitalizations on a weekly basis, too, and have for some time. It likely won’t be long before total hospitalizations from COVID-19 will eclipse total flu hospitalizations, and ICU admissions and deaths already have eclipsed flu numbers.
Seventeen percent of all cases ended up hospitalized – 32% ended up in critical care, and 19% ended up on a ventilator.
In a city-by-city breakdown, Dallas still comes in with the highest number of cases – 4,395, or 55.6%. Highland Park has 18 cases so far, and University Park has 26.
The county does not count recoveries because it’s not a variable being used nationally by the Centers for Disease Control and Prevention, nor by state health departments. However, one can extrapolate that the 83% of total cases that have not been hospitalized – at the very least – are on their way to recovery or have recovered, county officials explained recently.
“The exact number of patients who have been released from area hospitals to continue their recovery at home is not available at this time,” Lauren Trimble, Dallas County Judge Clay Jenkins’ chief of staff, said.
St. Marks Students Making PPE, But Need Help
 Members of the St. Mark’s robotics team and other students have banded together to provide frontline medical workers with face shields – but they need help.
Members of the St. Mark’s robotics team and other students have banded together to provide frontline medical workers with face shields – but they need help.
“We are providing hundreds of shields to non-profits and civic groups that we have identified in our community and we are also working with other schools, pooling our resources, to meet the growing needs of local and regional organizations,” the group said.
The group has distributed 3D printers to students’ homes, and those students are working “around the clock” to make more shields – but they could use supplies.
For details, and to contribute, see their sign-up page here.




Pingback:You Are Now Free To Move About the Country | People Newspapers